Lyme Disease and Tick Bite FAQs
By: Dr. Joseph Mechak
Summer brings sun, sand, pools, summer camps, and… ticks. Ticks get a bad name, and rightfully so at times. There is a lot of misinformation, incomplete information, and myths out there. We want to arm you with some reliable information and trustworthy references in case you cross paths with one of these little guys this summer.
What is Lyme Disease? – Lyme disease got it’s name after being discovered in Lyme, Connecticut in 1975. It is an infection caused by a bacteria called Borrelia burgdorferi. In the Mid-Atlantic region this bacteria is almost exclusively carried by the blacklegged deer ticks (ixodes scapularis). The infection is most commonly seen from late spring to early fall due to the life cycle of the tick. Signs and symptoms of Lyme disease include:
- Common/Early findings: Bullseye rash – Found in 70-80% of those infected, this is by far the most common and most specific finding of Lyme Disease. The rash is classically a spreading, circular, red rash that is shaped like a bullseye. This is usually, but not always, at the site of the bite and starts within 1-2 weeks. [see photo below]
- Less common/later findings: Joint pain and/or swelling, fatigue and malaise, low grade fever and chills, swollen lymph nodes
- Uncommon/late findings: one sided facial droop, severe headache, neck stiffness, heart palpitations, syncope (passing out).
How do we diagnose Lyme Disease? – In most cases, we can make the diagnosis by history and physical exam alone. There are also blood tests available but they can be difficult to interpret and not always accurate. The American Academy of Pediatrics (AAP) and CDC do not recommend performing tests on the tick to see if it carries the B. burgdorferi bacteria.
How do we treat Lyme Disease? – The good news about Lyme Disease is that it is usually very treatable. There are a few antibiotics that very effectively treat this infection, namely Doxycycline and Amoxicillin. In children with a high risk tick exposure (see more below) we may even start a preemptive antibiotic to thwart any infection from starting.
Do all ticks cause Lyme Disease? – No. There are about 6 types of human-biting ticks in Maryland. The Blacklegged Deer Tick (ixodes scapularis) is the only of these to transmit Lyme Disease.
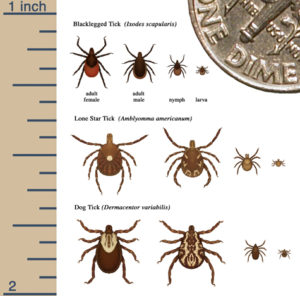
Most common ticks in Maryland – photo credit Maryland.gov Carroll County Health Department [CLICK TO ENLARGE]
Do all deer tick bites cause Lyme Disease? – No! Remember, Lyme disease is not actually caused by a tick bite. It is caused by a bacteria (B. burgdorferi) that is carried on the tick. Only about 30-50% of deer ticks in our region carry this bacteria.
Overall, only about 3% of all deer tick bites will cause Lyme Disease. Not all bites are created equally either! If a tick is attached for less than 36 hours, not engorged, and not buried in the skin, the risk of transmission is very, very low! On the other hand, a tick that has been feeding for more than 72 hours and is engorged, the risk is about 25%. These are the kind of exposures we may consider preventative antibiotics.
What is Chronic Lyme Disease? – Good question… the jury is still out about Chronic Lyme Disease. At this point, most medical professionals do not recognize Chronic Lyme as a diagnosis. There is still a lot of active research in the field and we continue to learn more every day.
How can I prevent Lyme Disease?
- Wear long sleeves, pants, hats, and socks during high risk activities like hiking or camping
- Apply DEET containing bug spray to skin and clothing (consult your doctor less than 6 months old)
- Consider treating clothing with permethrin if you in wooded or other high risk areas often
- Do ‘tick checks’ after your child is near fields or wooded areas. Ticks love crevasses so take extra care in areas like armpits, between the legs, in/near the hair, around the ears, and in the belly button
So, what should I do if my child is bitten by a tick?
- Take a deep breath. Remember, the risk of Lyme disease from a tick bite is actually very low, especially if it has been attached for less than 36 hours!
- Remove the tick, and make sure you get the whole thing. See these tips and tricks from the AAP and CDC for proper removal technique: Tick removal Tick Removal and testing
- Put the tick in a sealed bag or container so we can help identify it if needed
- Contact us by phone (301-279-6750), chat, or email (advicenurse@potomacpediatrics.com if:
- The tick was attached for more than 36 hours and engorged because your child may qualify for a preventative antibiotic dose
- You notice a bullseye rash
- You notice any of the other later/late signs/symptoms of Lyme Disease, regardless of a known tick bite
- If you have ANY questions or concerns!
————
For more information, visit these trusted websites:
HealthyChildren.Org – How to Remove a Tick
HealthyChildren.Org – Lyme Disease
CDC.gov – Lyme Disease










Leave a reply